The Truth About SSRI Antidepressants
What Everyone Needs to Know About Antidepressants
February 7, 2026
The public is at last awakening to the dirty secret of SSRI antidepressants—they trigger psychotic violence (e.g., suicides and sometimes mass shootings). This side effect was discovered in clinical trials but covered up by the FDA, even after the agency received a deluge of complaints (39,000 in the first nine years) once the first SSRI, Prozac, hit the market.
Because of those deaths, lawsuits through discovery found the drug companies were well aware of these issues (and many more) but chose to conceal them. As such, we now have a much clearer picture of the harms of these medications.
Note: while many patients react badly to SSRIs, there is also a subset of patients who benefit from them (discussed here). Sadly, it is quite rare that patients will work with antidepressant prescriber practitioners who have the time and knowledge to accurately determine which patients to give these drugs to.
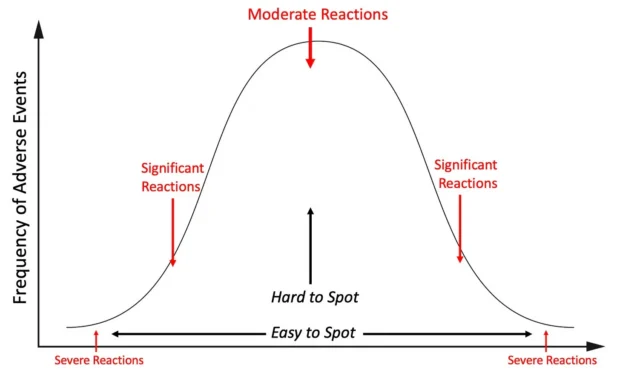
The Toxicology Bell Curve
In toxicology, you will typically see severe and extreme reactions occur much less frequently than moderate reactions:
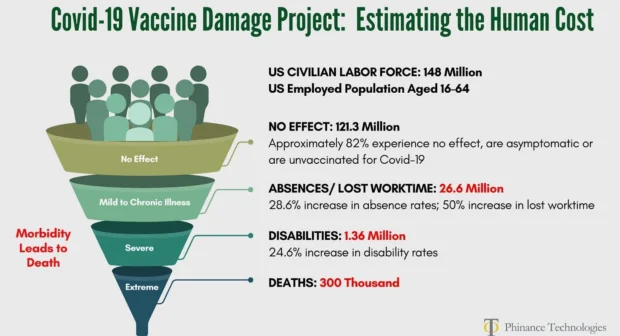
For example, consider the distribution of injuries from the COVID-19 vaccines.
Note: these calculations were based on 2023 data, and since then, vastly more evidence of harm has emerged (e.g., a recent poll found 63 million American adults had minor reactions to the vaccine and 17 million had severe side effects).
As such, violent psychosis is just the tip of the iceberg for the mild-altering effects SSRIs have. For example, in a survey of 1,829 patients on antidepressants in New Zealand:
• 62% reported sexual difficulties
• 60% felt emotionally numb
• 52% felt not like themselves
• 47% had experienced agitation
• 39% cared less about others
Most importantly, the respondents to that survey reported that their prescribers did not warn them about many of these side effects.
Doctored Data
Originally developed as a weight loss drug, Eli Lilly pivoted to having Prozac “treat” depression as this metric was subjective to the point any trial could be doctored to show a “benefit.” Despite this, Prozac’s initial data was so atrocious, it could only be approved through bribes (which a former Eli-Lilly executive testified occurred).
This fraud is proven by patients consistently choosing to stop taking SSRIs despite them being “proven” to make you feel better:
• A review of 29 published and 11 unpublished Paxil clinical trials containing 3704 patients who received Paxil and 2687 who received a placebo, an equal proportion of patients in both groups left their study early (suggesting Paxil’s benefits did not outweigh its side effects), and that compared to placebo, 77% more stopped the drug because of side effects and 155% more stopped because they experienced suicidal tendencies.
• A study of 7525 patients found that 56% of them chose to stop taking an SSRI within 4 months of being prescribed it.
• An international survey of 3,516 people from 14 patient advocacy groups found that 44% had permanently stopped taking a psychiatric drug due to its side effects.
• A survey of 500 patients found 81.5% were unsure if their anti-depressants were necessary.
Likewise, the Epoch times recently aired an insightful interview with a psychiatrist which highlighted that:
• The difference between patients taking antidepressants and placebos in trials is consistently very small, so creative ways are made to rearrange the data to conceal this.
• Forgotten research in the 1960s showed that the benefits of antidepressants disappeared when patients were given active (side-effect promoting) placebos, as those side effects made patients believe they were receiving a real antidepressant, and that provided the psychological motivation to get past their depression (which was corroborated by a forgotten 2004 Cochrane review).
Note: other authors have highlighted the lack of side effects with the inert placebos now used makes it very easy for investigators to identify who is taking the tested drug, at which point bias will inevitably emerge leading to them inflating their assessments of the subject psychological benefits those patients received.
• Members of the profession have repeatedly highlighted why antidepressants are an unproven therapy with real side effects, but their voices have been consistently ignored.
Note: fluorinated versions of pharmaceuticals tend to be more toxic and persist for longer periods in the body (making them much harder to detoxify from). Many believe a key reason SSRIs cause so many issues is due to the high dose of fluoride they bring into the brain.
Violent Behavior
In 1985 when the FDA’s safety reviewer scrutinized Eli Lilly’s Prozac application, they realized Lilly had “failed” to report psychotic episodes of people on the drug and that Prozac’s adverse effects resembled that of a stimulant drug. In turn, the warnings on the labels for SSRIs, such as anxiety, agitation, panic attacks, insomnia, irritability, hostility, aggressiveness, impulsivity, akathisia, hypomania, and mania match the effects commonly observed with stimulant street drugs such as cocaine and methamphetamine. Likewise:
• A Cochrane review found SSRIs were found to double the risk of suicide.
• A 2000 study of 20 volunteers in good mental health found Zoloft made 10% become suicidal (with one almost killing themselves)—both of whom remained deeply disturbed for months.
• Eli Lilly showed in 1978 that cats who had been friendly for years began to growl and hiss on Prozac and became distinctly unfriendly until Prozac was stopped.
Note: antidepressants were marketed on the basis “depression is a chemical imbalance” (brain serotonin deficiency) despite no evidence supporting this, and it is only in recent years this has begun being acknowledged. Furthermore, autopsy studies of individuals who committed suicide (e.g., this one and this one) found they actually had elevated brain serotonin levels—providing a potential mechanism to explain how SSRIs trigger suicide.
To illustrate what this can look like, I will share what four different patients experienced prior to killing themselves or others:
A month later, Toran experienced a severe cluster of adverse reactions including suicidal behavior, self-harm, aggression, hostility, hallucinations, lack of concentration and impaired functioning. The symptoms were so severe that he dropped out of school. His psychiatrist’s response was to increase his dose, which worsened the adverse reactions.
Six days later, Jake had his first reaction. He walked out of an exam half-way through it and cried for about 2-3 hours that night, saying, “You don’t know what it’s like in my head.” His parents thought this was from the stress of the exams. They never imagined that a drug could do this to a person.
The last two days she was just a complete zombie I have to say. She was just agitated, jumping at every noise and not making sense. I was very concerned. We were very close to Cecily. I just loved her deeply.
Shortly before his death, Woody came home crying after driving around all day. He sat in a fetal position on the kitchen floor profusely sweating with his hands pressing around his head saying, “Help me. Help me. I don’t know what’s happening to me. I am losing my mind. It’s like my head is outside my body looking in.”
Note: the process through which SSRIs do this (e.g., some individuals report an experience akin to “being possessed”) is discussed further here.
Fortunately, thanks to MAHA being elected to office, after decades, there at last appears to be real interest in addressing this issue. Consider, for example, this recent statement from H.H.S. Secretary Robert F Kennedy Jr:
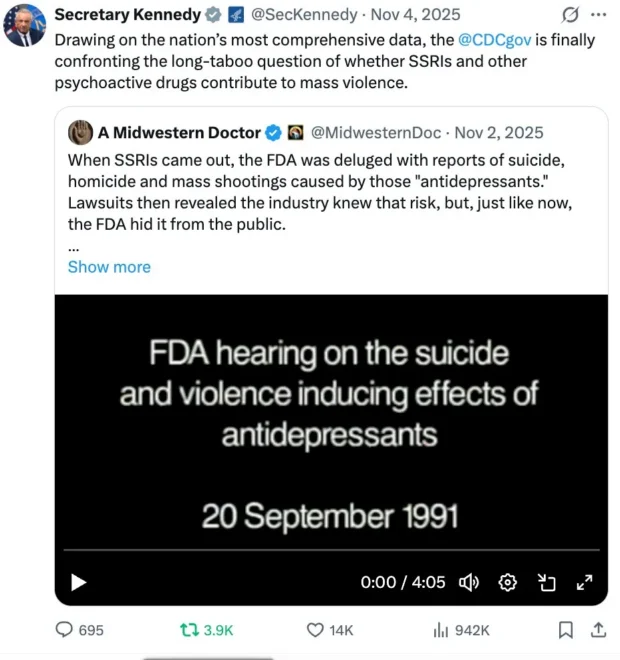
Note: initially, the media disclosed school shooters were on SSRIs, but then stopped ever mentioning a shooter’s medications. Recently, I learned through a CDC employee the CDC has found shooters continue to be on SSRIs but has avoided disclosing it to avoid the political ramifications of acknowledging this.
Likewise, the agitating quality of SSRIs can frequently trigger Bipolar disorder. For example:
• Yale researchers reviewing the records of 87,290 patients with depression or anxiety found SSRIs made 7.7% become bipolar each year (tripling the rate patients become bipolar).
• A survey found 60% of bipolar patients become bipolar after receiving SSRIs for depression.
• Peter Breggin reported that of 184 hospitalized patients started on an SSRI, 11 developed mania and 8 became psychotic, and in Yale, 8% of 533 consecutive admissions were for mania or psychosis caused by antidepressants, with two patients heard voices commanding them to kill themselves.
This helps to explain why bipolar has become hundreds of times more common since the pre-SSRI era and switched from being a temporary to lifelong condition that is far more disruptive and difficult to treat (e.g., 83% of bipolar patients reported being severely impaired in some facet of their lives).
Note: a good case can be made that many of the severe complications from bipolar disorder are a result of the medications used to treat it rather than the disease itself.
Copyright © A Midwestern Doctor