Key Findings For Data Through July 12th
- According to the CDC, 101 children age 0 to 14 have died from influenza, while 31 children have died from COVID-19.
- No evidence exists to support the theory that children pose a threat to educational professionals in a school or classroom setting, but there is a great deal of evidence to support the safety of in-person education.
- According to the CDC, 131,332 Americans have died from pneumonia and 121,374 from COVID-19 as of July 11th, 2020.
- Had the CDC used its industry standard, Medical Examiners’ and Coroners’ Handbook on Death Registration and Fetal Death Reporting Revision 2003, as it has for all other causes of death for the last 17 years, the COVID-19 fatality count would be approximately 90.2% lower than it currently is.
Abstract
 A Family Guide to Covi...
Best Price: $36.00
Buy New $20.00
(as of 04:01 UTC - Details)
The CDC has instructed hospitals, medical examiners, coroners and physicians to collect and report COVID-19 data by significantly different standards than all other infectious diseases and causes of death.
A Family Guide to Covi...
Best Price: $36.00
Buy New $20.00
(as of 04:01 UTC - Details)
The CDC has instructed hospitals, medical examiners, coroners and physicians to collect and report COVID-19 data by significantly different standards than all other infectious diseases and causes of death.
These new and unnecessary guidelines were instituted by the CDC in private, and without open discussion among qualified professionals that are free from conflicts of interest.
These new and unnecessary guidelines were additionally instituted despite the existence of effective rules for data collection and reporting, successfully used by all hospitals, medical examiners, coroners, and physicians for more than 17 years.
As a result, elected officials have enacted many questionable policies that have injured our country’s economy, our country’s educational system, our country’s mental and emotional health, and the American citizen’s personal expression of Constitutionally-protected rights to participate in our own governance.
This paper will present significant evidence to support the position that if the CDC simply employed their 2003 industry standard for data collection and reporting, which has been successfully used nationwide for 17 years; the total fatalities attributed to COVID-19 would be reduced by an estimated 90.2%, and questions would be non-existent regarding schools reopening and whether or not Americans should be allowed to work.
… It is very possible that state health departments have been instructed by the CDC to over-count COVID fatalities, cases, and hospitalizations
Is It Safe for Students & Teachers to Return to School?
While the current question gripping the nation is, ‘Should schools reopen in the fall?’ The crucial data available through the CDC, but not being actively promoted by the CDC, asks a different question, ‘Should schools have ever closed in the first place?’
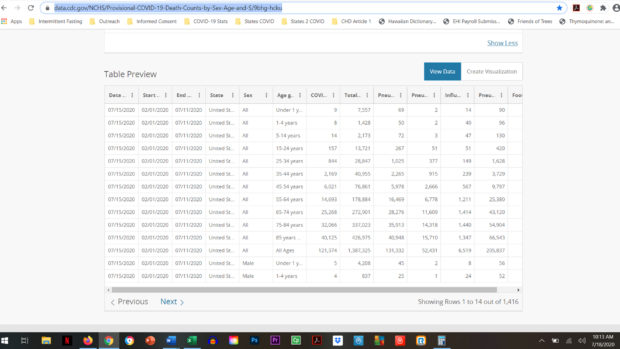
According to the CDC’s Provisional COVID-19 Death Counts By Sex, Age & State, we know the following data from Feb 1, 2020 through July 11th, 2020.1
- Three times as many children in the 0 to 14 age demographic have died from influenza (101) compared to COVID-19 (31).
- In the 0 to 14 age demographic, there have been 11,158 reported fatalities from all causes.
- Thus, COVID-19 fatalities in the 0 to 14 age demographic make up a very small 0.0278% of all fatalities.
 COVID-19: Lockdowns on...
Buy New $16.99
(as of 03:38 UTC - Details)
COVID-19: Lockdowns on...
Buy New $16.99
(as of 03:38 UTC - Details)
There is more data when looking at the 15 to 24 age demographic.
- 41.2% more teens and college age young adults, in the 15 to 24 age demographic, have died from pneumonia (267) compared to COVID-19 (157).
- In the 15 to 24 age demographic, there have been 13,721 reported fatalities from all causes.
- Thus, COVID-19 fatalities in the 15 to 24 age demographic make up only 1.14% of all fatalities.
We would not consider closing in-person educational institutions for typical seasonal flu or pneumonia fatalities, so why did we close them when COVID-19 numbers are even lower?
Some have argued for concern and caution in the 25 to 54 age demographic, which makes logical sense, so let’s look again at the current data available.
- More work force age adults, in the 25 to 54 age demographic, have died from pneumonia (9,268) compared to COVID-19 (9,034).
- In the 25 to 54 age demographic, there have been 146,663 reported fatalities from all causes.
- Thus, COVID-19 fatalities in the 25 to 54 age demographic make up 6.16% of all fatalities. The risk of fatality for COVID-19 is on par with the risk of fatality associated with contracting pneumonia, 6.32% in this age demographic.
As encouraging as this data is, we have concerns regarding data collection and reporting that we will discuss below that potentially lowers current fatality counts by 90.2%. It is very possible that state health departments have been instructed by the CDC to over-count COVID fatalities, cases, and hospitalizations, and we will present that evidence shortly.
… there is no more significant risk of fatality from contracting the SARS-CoV-2 virus than there is for developing pneumonia for teens & young adults.
As we have demonstrated in our first 2 research articles, ‘Are Children Really Recovering 99.9584% of the Time From COVID-19,’ and ‘COVID-19…Have You Heard? There Is Good News!’ there is a very real concern for Americans over the age 50 and especially over 65 years of age. Risk of fatality increases substantially for Americans over age 50 with at least 1 of the following comorbidities: Hypertension, Diabetes, Elevated Cholesterol, Kidney Disease, Dementia, Heart Disease. For perspective, according to the CDC, is the risk of dying from pneumonia higher than the risk of dying from COVID-19 in the 55 to 64 age demographic?
- Pre-retirement adults, in the 55 to 64 age demographic, had a slightly higher chance of dying from pneumonia (16,469) compared to COVID-19 (14,963).
 Unreported Truths abou...
Buy New $5.99
(as of 03:17 UTC - Details)
Unreported Truths abou...
Buy New $5.99
(as of 03:17 UTC - Details)
- In the 55 to 64 age demographic, there have been 178,884 reported fatalities from all causes.
- Since February 1st, fatalities in the 55 to 64 age demographic had a 12% greater risk of dying from pneumonia than COVID-19. COVID-19 fatalities in the 55 to 64 age demographic make up 8.21% of all fatalities and the risk of fatality due to COVID-19 is on par with the risk of fatality associated with contracting pneumonia, 9.21%.
The reported fatalities from the CDC’s Provisional COVID-19 Death Counts by Sex, Age & State webpage:
- Include ‘Probable’ fatalities, unconfirmed by testing, for COVID but not for influenza or pneumonia;
- Does not have accompanying data to detail how many of the fatalities had significant underlying, pre-existing, or comorbid medical conditions;
- Does not have accompanying data to determine if any of the fatalities were treated in a hospital setting and if the subsequent fatality was a result of the treatment.
What this data does reveal, however, is that there is no more significant risk of fatality from contracting the SARS-CoV-2 virus than from contracting influenza for children & teens. It also reveals that there is no more significant risk of fatality from contracting the SARS-CoV-2 virus than there is for developing pneumonia for teens & young adults.
We would not consider prohibiting in-person education when presented with infection rates and medical conditions at these rates, so why are we considering doing it for an infection that poses even less of a risk?
What this data reveals for adults working with children, teens, and young adults is that COVID-19 has a lower risk of fatality than pneumonia and the data suggests that other options should be created for both parents and educational professionals to allow them to choose which style of education they are currently comfortable with (1) traditional in-person education; (2) hybrid online/in-person education; or (3) virtual online education.
There are many questions that need to be addressed with the current situation.
Should each school district give parents and professionals options for in-person education, hybrid education, and/or online education this fall?
Should parents and professionals be allowed to decide where their comfort level is, and act accordingly given the data presented?
Or, should in-person students and professionals be forced to adhere to guidelines from the CDC that not only compromise the educational experience, but also place undue, unrealistic burdens upon them for something with a lower risk than pneumonia for all and influenza for the 0 to 14 age demographic?
We leave these questions for each American to answer.
 Remaking the American ...
Best Price: $12.55
Buy New $33.77
(as of 03:17 UTC - Details)
Remaking the American ...
Best Price: $12.55
Buy New $33.77
(as of 03:17 UTC - Details)
… (the) closure or not of schools had no measurable direct impact on the number of laboratory confirmed cases in school-aged children in Finland or Sweden.
More Scientific Evidence that It’s Safe for Children to Go Back to School
A genetic project in Iceland revealed interesting findings about children infecting adults.
“Children under 10 are less likely to get infected than adults and if they get infected, they are less likely to get seriously ill. What is interesting is that even if children do get infected, they are less likely to transmit the disease to others than adults. We have not found a single instance of a child infecting parents.”2
Sweden kept schools open with no demonstrative adverse impact upon children in school settings compared to Finland that elected to close in-person education.
“Sweden’s decision to keep schools open during the pandemic resulted in no higher rate of infection among its schoolchildren than in neighboring Finland, where schools did temporarily close, their public health agencies said in a joint report…In conclusion, (the) closure or not of schools had no measurable direct impact on the number of laboratory confirmed cases in school-aged children in Finland or Sweden.” 3
A German study found that children are unlikely vectors of COVID-19.
“Prof Reinhard Berner, the head of pediatric medicine at Dresden University Hospital and leader of the study, said the results suggested the virus does not spread easily in schools. “It is rather the opposite,” Prof Berner told a press conference. “Children act more as a brake on infection. Not every infection that reaches them is passed on.” The study tested 2,045 children and teachers at 13 schools — including some where there have been cases of the virus.” 4
No evidence of children infecting teachers in Australia.
“Our investigation found no evidence of children infecting teachers…In contrast to influenza, data from both virus and antibody testing to date suggest that children are not the primary drivers of COVID-19 spread in schools or in the community.” 5
School environments are low risk and in-person education resuming should begin.
“Our report includes both the primary and secondary school setting, with no transmission in either setting. The limited evidence of transmission in school settings supports the re-opening of schools as part of the easing of current restrictions. There are no zero risk approaches, but the school environment appears to be low risk.” 6
Infected children do not spread the virus to other children, teachers or administrators.
“The main new finding is that the infected children did not spread the virus to other children or to teachers or other school staff…there was no secondary transmission of the virus to other children at the school, or from children to teachers.” 7
After all, based upon the July 11th data from the CDC’s Provisional COVID-19 Death Counts by Sex, Age & State webpage, if COVID-19 is an epidemic (122,374 Fatalities), then shouldn’t pneumonia (131,372 Fatalities) also be an epidemic?
Why Did the CDC Decide to Create Unique Reporting Rules for COVID-19 When Successful Reporting Rules Already Existed?
A double standard exists for how COVID-19 data is collected and reported versus all other infectious diseases and causes of death. Let’s examine three essential data categories; Fatalities, Cases & Hospitalizations for all infectious diseases because there are significant flaws in what constitutes a COVID-19 case, hospitalization and fatality.
On March 24th, the CDC decided to ignore universal data collection and reporting guidelines for fatalities in favor of adopting new guidelines unique to COVID-19. The guidelines the CDC decided against using have been used successfully since 2003.
After all, based upon the July 11th data from the CDC’s Provisional COVID-19 Death Counts by Sex, Age & State webpage, if COVID-19 is an epidemic (122,374 Fatalities), then shouldn’t pneumonia (131,372 Fatalities) also be an epidemic?1
Fatality Data
It is important to note that COVID-19 data is collected and reported by a much different standard than all other infectious diseases and causes of death data. This unique standard for COVID-19 was used, despite the existence of guidelines that have been successfully used since 2003 for data collection across all infective, comorbid, and injurious situations.
… the rules for coding and selection of the underlying cause of death are expected to result in COVID19 being the underlying cause more often than not.
This begs the question, if the CDC already has well established guidelines for reporting fatalities then why make up new guidelines for COVID-19?
COVID-19 data is collected and reported based upon the March 24th National Vital Statistics Systems (NVSS) Guidelines and the April 14th CDC adoption of a position paper authored by the Council of State and Territorial Epidemiologists (CSTE). 8,9
However, the data for all other causes of death is based upon the 2003 CDC’s Medical Examiners’ & Coroners’ Handbook on Death Registration and Fetal Death Reporting and the CDC’s Physicians’ Handbook on Medical Certification of Death. 10,11
On March 24th, the NVSS, under the direction of the CDC and National Institute of Health (NIH), instructed physicians, medical examiners, and coroners that COVID-19 would:
- be recorded as the underlying cause of death “more often than not;”
- be recorded as the cause of death listed in Part I of the death certificate even in assumed cases;
- be recorded as the primary cause of death even if the decedent had other chronic comorbidities. All comorbidities for COVID-19 would be listed now in Part II, rather than in Part I as they had been since 2003 for all other causes of death.
March 24th, 2020 – NVSS COVID-19 Alert No. 2
“Will COVID-19 be the underlying cause? The underlying cause depends upon what and where conditions are reported on the death certificate. However, the rules for coding and selection of the underlying cause of death are expected to result in COVID19 being the underlying cause more often than not.”
“Should “COVID-19” be reported on the death certificate only with a confirmed test? COVID-19 should be reported on the death certificate for all decedents where the disease caused or is assumed to have caused or contributed to death. Certifiers should include as much detail as possible based on their knowledge of the case, medical records, laboratory testing, etc. If the decedent had other chronic conditions such as COPD or asthma that may have also contributed, these conditions can be reported in Part II. (See attached Guidance for Certifying COVID-19 Deaths)”
It’s worth noting that Part I of a death certificate is the immediate cause of death listed in sequential order from the official cause on line item (a) to the underlying causes that contributed to death in descending order of importance on line item (d), while Part II is/are the significant conditions NOT relating to the underlying cause(s) in Part I.
As we will demonstrate shortly, comorbid conditions are always listed on Part I of death certificates as causes of death per the 2003 CDC Handbook, so that accurate reporting can be developed. Comorbidities are seldom placed in Part II, as this is typically the place where coroners and medical examiners can list recent infections as underlying factors.
Prior to the March 24th and April 14th decisions, any comorbidities would have been listed in Part I rather than Part II and initiating factors, like recent infections, would have been listed on the last line in Part I or in Part II.
Why does this matter?
This matters because the Part I causes of death are statistically recorded for public health reporting, while Part II does not hold nearly the same statistical significance in reporting. This March 24th NVSS guideline essentially allows COVID-19 to be the cause of death when the actual cause of death should be the comorbidity according to the industry-standard 2003 CDC Handbook. It can be a bit confusing, so we will present an example shortly for clarity.
On April 14th, the CDC in conjunctions with approval from the National Institute of Health (NIH), adopted the CSTE position paper that authorized the following guidelines for data collection and reporting which are completely unique for COVID-19 and had never been done before which:
- allowed for ‘Probable’ cases, hospitalizations, and fatalities [section A5];
- created a pathway for the minimum standards of evidence to be a single cough [section A1];
- created a pathway for completely bypassing laboratory testing in order to classify a COVID-19 case as positive [section A5];
- created a pathway for the minimum standard of evidence necessary for determining a COVID-19 case to be positive as being within 6 feet of a ‘Probable’ case for 10 minutes or traveling to an area with outbreaks [section A3];
- declined to create any methodology for ensuring the same COVID-19 positive person would not be counted multiple times as a new case upon being tested multiple times [section B].
April 14th, 2020 – CDC Adopts CSTE Interim-20-ID-01
Title: Standardized surveillance case definition and national notification for 2019 novel coronavirus disease (COVID-19)
“VII. Case Definition for Case Classification
- Narrative: Description of criteria to determine how a case should be classified.
A1. Clinical Criteria At least two of the following symptoms:
- fever (measured or subjective), chills, rigors, myalgia, headache, sore throat, new olfactory and taste disorder(s) OR
- At least one of the following symptoms: cough, shortness of breath, or difficulty breathing OR
- Severe respiratory illness with at least one of the following:
- Clinical or radiographic evidence of pneumonia, or
- Acute respiratory distress syndrome (ARDS). AND
- No alternative more likely diagnosis
A2. Laboratory Criteria Laboratory evidence using a method approved or authorized by the FDA or designated authority:
Confirmatory laboratory evidence:
- Detection of SARS-CoV-2 RNA in a clinical specimen using a molecular amplification detection test
Presumptive laboratory evidence:
- Detection of specific antigen in a clinical specimen
- Detection of specific antibody in serum, plasma, or whole blood indicative of a new or recent infection*
*serologic methods for diagnosis are currently being defined
A3. Epidemiologic Linkage One or more of the following exposures in the 14 days before onset of symptoms:
- Close contact** with a confirmed or probable case of COVID-19 disease; or
- Close contact** with a person with:
- clinically compatible illness AND
- linkage to a confirmed case of COVID-19 disease.
- Travel to or residence in an area with sustained, ongoing community transmission of SARS-CoV2.
- Member of a risk cohort as defined by public health authorities during an outbreak.
**Close contact is defined as being within 6 feet for at least a period of 10 minutes to 30 minutes or more depending upon the exposure. In healthcare settings, this may be defined as exposures of greater than a few minutes or more. Data are insufficient to precisely define the duration of exposure that constitutes prolonged exposure and thus a close contact.
A4. Vital Records Criteria A death certificate that lists COVID-19 disease or SARS-CoV-2 as a cause of death or a significant condition contributing to death.
A5. Case Classifications
Confirmed:
- Meets confirmatory laboratory evidence.
Probable:
- Meets clinical criteria AND epidemiologic evidence with no confirmatory laboratory testing performed for COVID-19.
- Meets presumptive laboratory evidence AND either clinical criteria OR epidemiologic evidence.
- Meets vital records criteria with no confirmatory laboratory testing performed for COVID19.
- Criteria to distinguish a new case of this disease or condition from reports or notifications which should not be enumerated as a new case for surveillance
- N/A until more virologic data are available”
Additionally, the CSTE position paper gave no definition as to what constitutes a COVID-19 recovery for all state and country health departments to follow.
While the, seemingly independent, CSTE position paper was authored by five accomplished professionals from the Idaho, Alabama, Michigan, Hawaii, and Iowa state health departments; 5 of the 7 Subject Matter Experts who contributed to the position paper were directly employed by the CDC which raises ethical concerns about conflicts of interest.
It stands to reason that each of the professionals who contributed to the CSTE position paper were aware of the existence of the 2003 guidelines for reporting fatalities. Additionally, no subject matter experts from universities, medical examiners, coroners or private industry appear to have been consulted on the production of this highly questionable document.
So, why does all of this matter?
It matters for several reasons:
- The minimum standards defy accepted professional standards for differential diagnosis in medical practice;
- Section A3 empowers contact tracers, who are unlikely to have any medical training, to illegally diagnose patients without even examining them, which is a violation of medical law in every state and constitutes practicing medicine without a license;
- The CSTE position paper opens the door for any fatality to be listed as COVID-19 without any reasonable standard of evidence, while mandating that comorbidities simultaneously be deemphasized and moved to Part II, so as not to appear as a cause of death;
- Simultaneous testing for all other infectious diseases, with similar respiratory symptom profiles like Coccidioidomycosis for Valley Fever, is not required. We therefore have no clinical or statistical means of knowing if a co-infection was present along with a positive finding of the SARS-CoV-2 virus in the differential diagnosis process.
Why was all of this necessary with a successful methodology for physicians, medical examiners, and coroners already in place since 2003?
The CDC’s 2003 Handbook suggests that COVID-19 should be listed either at the bottom of Part I or in Part II of a death certificate, rather than as the top line item in Part I, despite Dr. Fauci’s describing in multiple press interviews, that medical examiners and coroners would not be doing this, which disregards any knowledge of the March 24th orders by the NVSS to do so.
The ability for medical examiners and coroners to register their best medical opinion was neutered by the March 24th NVSS guidelines.
Let’s review what would have happened had the CDC decided to use their 2003 Handbook rather than adopting new rules for COVID-19 reporting.
2003 – CDC Medical Examiners’ and Coroners’ Handbook on Death Registration
“Because statistical data derived from death certificates can be no more accurate than the information provided on the certificate, it is very important that all persons concerned with the registration of deaths strive not only for complete registration, but also for accuracy and promptness in reporting these events.”.
“The principal responsibility of the medical examiner or coroner in death registration is to complete the medical part of the death certificate.”
“The cause-of-death section consists of two parts. Part I is for reporting a chain of events leading directly to death, with the immediate cause of death (the final disease, injury, or complication directly causing death) online (a) and the underlying cause of death (the disease or injury that initiated the chain of events [SARS-CoV-2 in this case] that led directly and inevitably to death) on the lowest used line. Part II is for reporting all other significant diseases, conditions, or injuries that contributed to death but which did not result in the underlying cause of death given in Part I.”
Under these guidelines, the highest COVID-19 could be listed in the presence of an established comorbidity would be Part I, line item (d) or lower, or in Part II.