The State-Medical Complex
December 13, 2004
Diagnosis: Corruption
by Bill Sardi by Bill Sardi
The Federal branches of government responsible for protecting and promoting public health are in a state of moral collapse. The recent recall of the anti-inflammatory drug Vioxx, with the revelation that the continued use of the drug long after the Food & drug Administration and its manufacturer knew it doubled the risk of heart attacks and may have caused 30,000 or so avoidable deaths, is only a small picture of what is going on inside federal health agencies today.
The annual Federal budget is around $2.294 trillion. About $800 billion of that is defense spending (about half of that figure is hidden and doesn’t appear on the budget pie charts) For comparison, the combined 2004 budgets for three federal health organizations, the National Institutes of Health ($28.5 billion), the Centers for Disease Control ($4.8 billion), and Food & Drug Administration ($1.7 billion, including $300 million in user fees from pharmaceutical companies), represent a relatively small portion of the Federal annual spending. But more money won’t fix what’s wrong with Federal health agencies. In fact, it is money that has corrupted these once respected public agencies.
Here’s what these agencies claim they are doing for you.
According to the above chart, research in the prevention and treatment of cardiovascular disease, supported by the National Institutes of Health, has helped to save over 800,000 lives annually. Elias Zerhouni, MD, Director, National Institutes of Health (NIH), in his April 8, 2003 presentation before the 108th Congress to support 2004 budget requests, said: "We supported research that led to strategies as simple and inexpensive as taking aspirin to prevent heart disease and stroke"…. and "we also continue to evaluate the best therapeutic strategies in medical practice" including cholesterol-lowering trials and other studies that "showed that hypertension can be effectively managed with an initial choice of an inexpensive drug." What Dr. Dr. Zerhouni was talking about was a report issued in 1993 showing that an inexpensive diuretic (water pill) can significantly reduce the risk of stroke and death from high blood pressure.
But there is a problem with Dr. Zerhouni’s claims. Diuretics were recommended in practice guidelines, but numerous studies indicate physicians largely ignored the advice to use diuretics as first-line treatment for high blood pressure. The NIH-sponsored studies didn’t significantly change the percentage of patients receiving diuretics. [Am J Med113:52—8, 2002; Clin Therapy 24:1451—62, 2002; Value Health 6:18—28, 2003] Norwegian health authorities claim the NIH-sponsored studies were "unfit as a basis for general guidelines in the treatment of high blood pressure in Norway." [Tidsskr Nor Laegeforen 124:1419—20, 2004]. To show what a mess the practice of medicine is in today, one study showed that physicians were more likely to select a drug for hypertension based upon the supply of free samples provided by pharmaceutical representatives rather than the NIH study. [J Gen Intern Med 18:977—83, 2003]
Look carefully at the above chart provided by the NIH. The use of aspirin wasn’t recommended by the American Heart Association till 1993. Shortly thereafter the NIH sponsored-studies recommended diuretics over other more expensive blood pressure medications, but the use of diuretics did not significantly rise. Furthermore, the first statin cholesterol-lowering drug (Mavacor) was not introduced till late 1987. The dramatic drop in cardiovascular mortality rates occurred prior to the recommendations to use aspirin, diuretics or cholesterol-lowering drugs.
 What happened, starting in 1970, which would have caused such a dramatic drop in cardiovascular mortality? Cigarette use per capita per year began to decline from 4000 to 2000 in the period from 1970 to 2000 but the number of smokers (about 40+ million) remained about the same due to gradual increases in the size of the population and the number of cigarettes consumed per day per smoker remained about the same. It is difficult to pin down what caused the dramatic drop in cardiovascular disease mortality. It wasn’t due to anything doctors were prescribing.
What happened, starting in 1970, which would have caused such a dramatic drop in cardiovascular mortality? Cigarette use per capita per year began to decline from 4000 to 2000 in the period from 1970 to 2000 but the number of smokers (about 40+ million) remained about the same due to gradual increases in the size of the population and the number of cigarettes consumed per day per smoker remained about the same. It is difficult to pin down what caused the dramatic drop in cardiovascular disease mortality. It wasn’t due to anything doctors were prescribing.
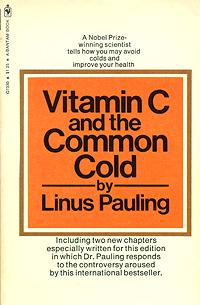
In 1970 Linus Pauling’s book, Vitamin C and The Common Cold, was published. From a statistical standpoint, the daily dietary consumption of vitamin C remained about the same over the past half century. But a significant number of people began taking vitamin C pills to supplement their diet. Pauling may have prolonged the lives of millions with the publication of his book.
 NIH scientists today continue to maintain that taking more than 200 milligrams of vitamin C per day is worthless because any amount beyond the 200 mg consumption point is excreted in the urine and will not raise blood concentrations. [Biofactors 15:71—4, 2001] But a recent analysis of nine pooled studies involving vitamin C shows that those people who consume more than 700 milligrams per day experience about a 30 percent reduction in cardiovascular disease mortality compared to non-vitamin pill users. [Am J Clinical Nutrition 80:1508—20, 2004] Consumers can’t even find a pill today that provides less than 500 milligrams of vitamin C. What do the consumers and vitamin manufacturers know that the NIH refuses to acknowledge?
NIH scientists today continue to maintain that taking more than 200 milligrams of vitamin C per day is worthless because any amount beyond the 200 mg consumption point is excreted in the urine and will not raise blood concentrations. [Biofactors 15:71—4, 2001] But a recent analysis of nine pooled studies involving vitamin C shows that those people who consume more than 700 milligrams per day experience about a 30 percent reduction in cardiovascular disease mortality compared to non-vitamin pill users. [Am J Clinical Nutrition 80:1508—20, 2004] Consumers can’t even find a pill today that provides less than 500 milligrams of vitamin C. What do the consumers and vitamin manufacturers know that the NIH refuses to acknowledge?
Next: The Centers For Disease Control
Here’s what happening this year’s flu season. There is a shortage of flu vaccine due to contamination at a major vaccine manufacturing plant. Instead of 100 million Americans getting a flu shot as planned, only about 61 million doses are available. Despite concerns that there might be a major flu epidemic without adequate vaccination, the flu season is off to a very slow start. Here’s what the flu charts look like without adequate vaccination.
The flu chart is a bit misleading. For example, flu activity in Delaware, the first state to be classified as having widespread flu problems, is in the red zone because confirmed cases have been reported in every county of the state. But the state has only three counties and just six flu cases in all.
It turns out this year’s prevalent flu strain, A-Wellington, is not included in this year’s flu shot. The 2004-05 version of the flu vaccine is about 2/3rds less effective in activating antibodies against A-Wellington than it is against last year’s A-Fujian strain. Flu vaccines confer some protection against viruses if they are similar and the A-Fujian and A-Wellington are both H3N2 types of influenza viruses. However, a study showed that last year’s flu shots were only effective in 5 of 10 healthy adults and only 4 of 10 high-risk adults. Americans are doing far better this year, so far, without much help from the CDC.
Now for the FDA
If you think the list of unsafe drugs is limited to what Dr. David Graham revealed in Congress, five more drugs in addition to Vioxx (Bextra, Accutane, Crestor, Meridia and Serevent), you had better think twice. There are more drugs than these that are unsafe. If you or your loved ones take prescription drugs, you need to know which ones are unsafe from an unbiased source (not the FDA).
Ralph Nader’s Public Citizen Group has been publishing a list of "do not use" drugs for some time now and has a good track record at predicting which approved drugs will be recalled two years before they are actually withdrawn. Worst Pills, Best Pills is a monthly newsletter available electronically through Public Citizen’s Web site. There are 100,000 deaths a year in the United States from adverse reactions from properly-used medications, and nearly 1.5 million people are injured so seriously by adverse drug reactions that they require hospitalization. Citizens can subscribe to WorstPills.org for a $15 fee, which includes a monthly newsletter with additional electronic updates and news on dangerous prescription drugs.
For example, Public Citizen reports that the rate of kidney failure or damage among patients taking the cholesterol drug Crestor is 75 times higher than in patients taking all other statin drugs. Public Citizen has renewed its call for the drug to be taken off the market. Officials for the manufacturer of Crestor have been quoted as saying: “We have been assured today at senior levels in the FDA that there is no concern in relation to Crestor’s safety.” That’s what was said about Vioxx.
Dr. Sandra Kweder, deputy director at the Office of New Drugs at the FDA, said that she did not agree with Graham’s assessment with the risk posed by the five drugs singled out by Graham. Kweder maintains the FDA’s drug review process is the "gold standard" for the industry, but after Graham disclosed his list of drugs that pose an avoidable increased risk to the news media, the FDA took action to tighten controls on one of them (Accutane). It’s an admission the FDA is covering for the drug manufacturers. The $300 million user fees drug companies provide the FDA is being used to protect the drug companies, not consumers.
We can’t forget, while people were needlessly dying from the use of Vioxx, the FDA took Dr. Graham to task for violating procedural guidelines by airing his data to the British Medical Journal, where the world could inspect the data the FDA had been hiding. In November of 1996 Merck scientists had hypothesized that patients taking Vioxx would have higher rates of heart disease compared to taking aspirin and by 1998 they knew that Vioxx disabled one of the body’s defenses against the clumping of blood platelets in arteries. Graham said that before the FDA approved Vioxx, Merck performed a study that found nearly a sevenfold increase in heart attack risk with low doses of Vioxx. A change in the Vioxx label took 18 months to gain approval, and it was not categorized as a “warning.” Dr. Graham had been fighting inside the FDA for some time before he skipped around procedural guidelines and disclosed what was going on inside the FDA.
The same people are still in charge at the FDA today. Nobody has been fired. In the mid-1990s only 2 percent of new drugs were approved by the FDA. Today 68 percent of new drugs are approved in the United States. Safeguards have been dismantled. The time it takes to get a drug approved has been shortened, but drug costs remain high, despite the fact that the pharmaceutical companies continue to maintain their R & D costs are what drive up consumer prices for drugs.
Steven Galson, MD, acting director of the FDA’s Center for Drug Evaluation and Research, said Graham’s congressional testimony “does not reflect the views of the agency.” In fact, when Dr. Graham said the country is "virtually defenseless" against a repeat of the Vioxx fiasco, Galson immediately rejected that, saying it had "no basis in fact." The voluntary Merck recall throws Galson’s defense to the wind and now shames the entire FDA.
